Bacterial vaginosis vs. yeast infection

Reviewed by Steve Silvestro, MD, Ro,
Written by Chimene Richa, MD
last updated: Apr 21, 2021
5 min read
Here's what we'll cover
You’re itchy, you’re uncomfortable, and you know something isn’t right down there. But before you go self-diagnosing, consider the following: bacterial vaginosis and yeast infections are two common vaginal conditions that tend to present with similar symptoms. However, each requires different treatments. Here’s how to tell the difference between the two and how to treat them.
What are bacterial vaginosis and yeast infections?
Bacterial vaginosis (BV) is a condition that occurs when something disrupts the vagina’s natural bacterial balance, also called vaginal flora. The microorganisms that live in the vagina are necessary for maintaining normal vaginal pH and the healthy status quo. They also take up space to ensure invaders can’t settle there. When the balance goes awry, you can have an overgrowth of “bad” kinds of bacteria called anaerobes. This overgrowth can sometimes lead to vaginal inflammation or vaginitis (Kairys, 2020).
A vaginal yeast infection, also known as vaginal candidiasis, is caused by a species of fungus (yeast is a form of fungus) called Candida; specifically, Candida albicans (C. albicans) is the most common culprit. This yeast is typically present inside the body, but it’s usually kept in check by your immune system and the presence of “good bacteria. If the environment of your vagina changes, it can become particularly hospitable to this yeast, sometimes resulting in infection (Jeanmonod, 2020).
BV and yeast infections have similar symptoms and can be tough to tell apart. Let’s talk about the symptoms, causes, and treatments for each of these vaginal conditions.
Bacterial vaginosis (BV)
Symptoms of BV
Bacterial vaginosis is the most common cause of vaginal discharge. It is estimated that approximately 30 percent of women in the U.S. between the ages of 14-49 may experience this condition (Kairys, 2020). The resulting inflammation usually isn’t dangerous, and at least half of people who develop BV don’t even experience noticeable symptoms (Hay, 2014). But when the symptoms do become apparent, they can be unpleasant. A few of the signature symptoms include (Kairys, 2020):
A “fishy” odor, before or after adding potassium hydroxide (KOH), also called the whiff test
Thin, grayish white vaginal discharge
Vaginal itching
A burning sensation with urination
Pain during sex
Causes of BV
For bacterial vaginosis to occur, something typically has to disrupt the vagina’s natural bacterial balance. When everything is at it should be, the “good” bacteria (lactobacilli) outnumber the “bad” bacteria (anaerobes). But if something comes along and disrupts the vaginal environment, BV can develop. Some of the risk factors associated with bacterial vaginosis include (Sobel, 2020):
Douching or excessive cleaning of the vagina
Hormonal changes that accompany events like menstruation, pregnancy, and menopause
Sex with male or female partners
Presence of sexually transmitted infections, like herpes and HIV
Cigarette smoking
Treatments for BV
The primary goal of treatment in people with BV is to relieve their symptoms; however, it can get better without treatment in up to one-third of people. If you suspect that you may have bacterial vaginosis, see your healthcare provider for a physical exam, including a pelvic exam, and to discuss treatment options (Sobel, 2021-a).
BV treatment typically involves prescription medications like metronidazole (brand name Flagyl), clindamycin (brand name Cleocin), tinidazole (brand name Tindamax), and secnidazole (brand name Solosec). Some people turn to probiotics to help with their BV. In truth, there is not enough information to recommend for or against the use of probiotics for BV; more research is needed in this area. Approximately 30–50% of people will have a recurrence of their bacterial vaginosis after completing treatment (Sobel, 2021-a). You should avoid having sex, using tampons, sex toys, etc., during treatment.
Yeast infections
Symptoms of vaginal yeast infections
Like BV, vaginal yeast infections are common—almost three out of four women experience them at some point in their lives. The symptoms can appear similar to those of BV and include (Jeanmonod, 2020):
Itching, burning, and/or irritation of the vagina and vulva
Soreness
Thick, white vaginal discharge that’s odor-free and resembles cottage cheese
A burning sensation with urination and/or sex
Redness and swelling of the vulva and vagina
It’s important to know that BV isn’t considered a sexually transmitted infection (STI), although it is associated with sexual activity. Your sexual partner doesn't necessarily need treatment if you have BV. Bacterial vaginosis also puts you at an increased risk of getting STIs, like herpes, HIV, etc.
Causes of yeast infections
While yeast infections differ from bacterial vaginosis, some of the root causes overlap. Your vagina naturally contains different types of yeast. The good bacteria we discussed earlier—lactobacilli—typically keep it in check. When something disrupts that delicate balance of bacteria, it can create an overgrowth of one specific type of yeast called Candida. Some of the risk factors for this imbalance include (Jeanmonod, 2020):
Birth control pills or hormone therapies that affect estrogen levels
Antibiotic use
Uncontrolled diabetes
Pregnancy
Immune system problems
Treatments for yeast infections
Candida species can live in the vagina and not cause symptoms—this is the case 10-20% of the time. These people generally do not need treatment. Like BV, the main purpose of treating most yeast infections is symptom improvement (Sobel, 2021-b).
In many cases, you can treat yeast infections with over-the-counter (OTC) vaginal creams or suppositories like clotrimazole (brand name Gyne-Lotrimin) or miconazole (brand name Monistat). Alternatively, your healthcare provider can prescribe a single dose of an oral antifungal medication, like fluconazole (brand name Diflucan) (Sobel, 2021-b).
If you have a severe infection or you’re experiencing recurrent infections (more than four per year), you may need to be on prescription medicines for longer than a single dose. It’s best to avoid vaginal intercourse during your treatment and steer clear of inserting anything into your vagina that could harbor bacteria, like tampons, menstrual cups, and sex toys (Sobel, 2021-b).
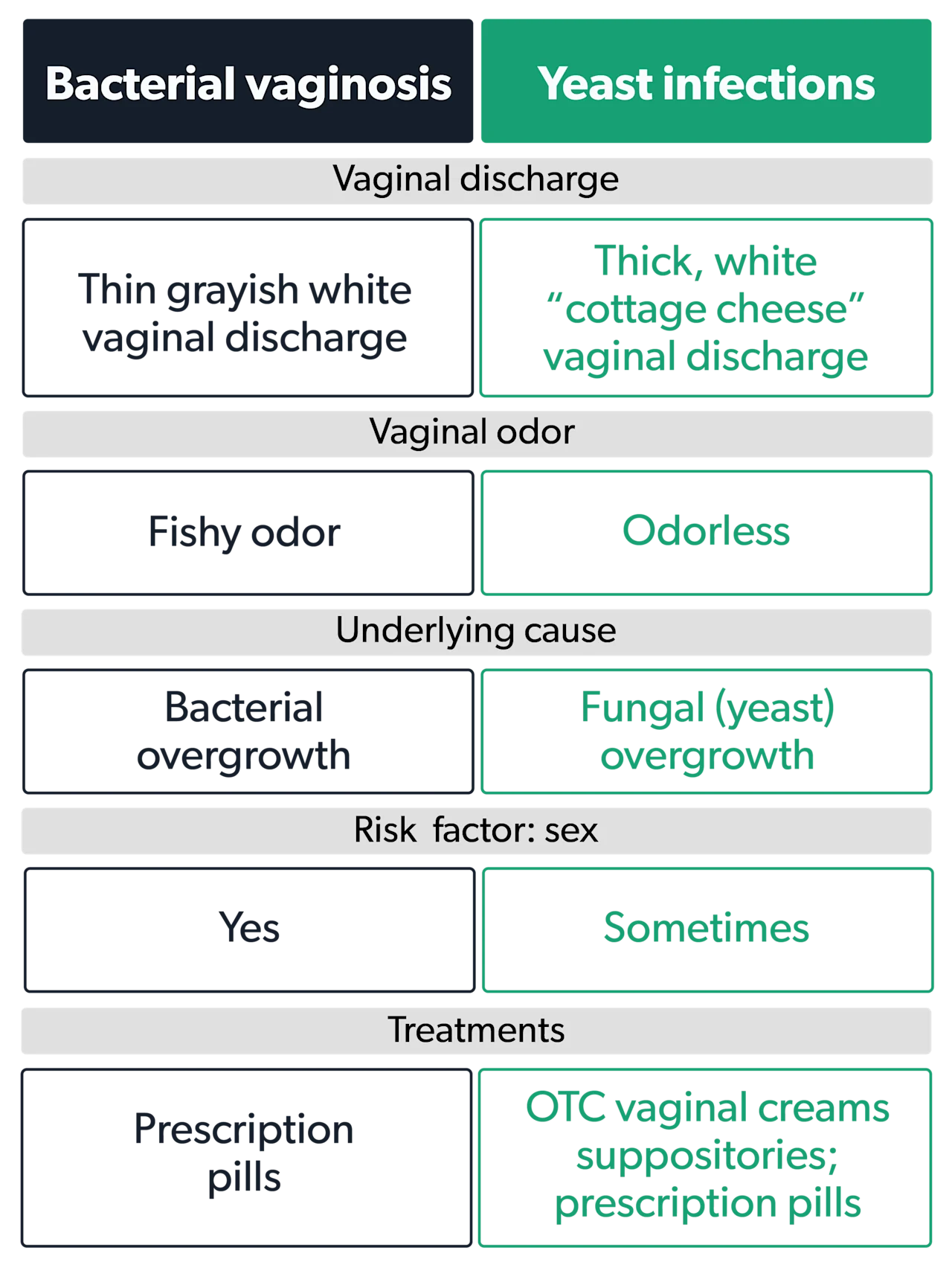
Bacterial vaginosis vs. yeast infections
It can sometimes be challenging to tell if your vaginal infection is due to bacterial vaginosis or a yeast infection; your healthcare provider can help you differentiate between the two. Here is a summary of the main characteristics of these two vaginal conditions.
Tips for preventing BV and yeast infections
While the treatments may differ, the prevention strategies for avoiding BV and yeast infections overlap. The key objective is to maintain the natural bacterial balance of your vagina. Here are some ways to do that:
Always wipe from front to back in the bathroom.
Don’t douche.
Wear cotton underwear that’s not too tight and wicks away moisture.
Avoid long, hot baths and too much time in hot tubs.
Don’t use scented feminine products.
If you go for a sweaty workout or swim, change out of wet clothes ASAP.
Keep your diabetes under control.
When to see a healthcare provider
Without a pelvic exam, it can be tough to know if you have BV or something else. If you have vaginal discharge that comes with an odor or if you develop a fever, it’s time to make an appointment.
Another reason to see your provider is if you have multiple sex partners or recently started having sex with someone new and now have vaginal symptoms. Sometimes the symptoms of BV can resemble those of sexually transmitted infections. And finally, if you thought you had a yeast infection but the OTC remedies just aren’t working, get medical advice.
While you can usually treat yeast infections with OTC medications, some instances merit an office visit.
Suppose it’s your first yeast infection ever. In that case, you may want to consult with your healthcare provider to make sure you’re not experiencing another issue that requires different treatment, like a urinary tract infection (UTI) or an STI. You should also seek medical attention if you get a yeast infection while pregnant, since not all OTC meds are pregnancy-safe. And finally, if you get yeast infections a lot (four or more per year), you may need longer-term treatment.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Hay, P. (2014). Bacterial vaginosis. Medicine, 42 (7) (2014), pp. 359-363. doi:10.1016/j.mpmed.2014.04.011. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S1357303914001121
Jeanmonod R, Jeanmonod D. (2020 Nov). Vaginal Candidiasis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK459317/
Kairys N, Garg M. (2020 Nov). Bacterial Vaginosis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK459216/
Sobel, J.D. & Mitchell, C. (2020 Sept). Bacterial vaginosis: Clinical manifestations and diagnosis. In Barbieri, R.L. & Eckler, K. (Eds.) Retrieved from https://www.uptodate.com/contents/bacterial-vaginosis-clinical-manifestations-and-diagnosis
Sobel, J.D. (2021-a March). Bacterial vaginosis: Treatment. In Barbieri, R.L. & Eckler, K. (Eds.) Retrieved from https://www.uptodate.com/contents/bacterial-vaginosis-treatment
Sobel, J.D. (2021-b March). Candida vulvovaginitis: Treatment. In Barbieri, R.L., Kauffman, C.A., & Eckler, K. (Eds.) Retrieved from https://www.uptodate.com/contents/candida-vulvovaginitis-treatment










